Connect With Us
Blog

Causes of a Broken Toe and When to See a Podiatrist

A broken toe can result from various causes, including direct trauma, stubbing the toe against a hard surface, or dropping a heavy object on the foot. Sports injuries, accidents, and even sudden, forceful movements can also lead to a toe fracture. Common symptoms include severe pain, swelling, bruising, and difficulty walking. While minor fractures may heal with rest and home care, it is important to know when to call a podiatrist. Seek medical attention if there is intense pain, visible deformity, numbness, or if the toe is cold or pale, indicating poor blood flow. Persistent swelling and an inability to move the toe also warrant a professional evaluation. Early diagnosis and appropriate treatment is vital to prevent complications and ensure proper healing of a broken toe. If you have any of the above symptoms and believe you may have fractured your toe, it is suggested that you seek prompt attention from a podiatrist who can diagnose and treat broken toes.
Broken toes may cause a lot of pain and should be treated as soon as possible. If you have any concerns about your feet, contact Daniel Bell, DPM from Florida. Our doctor will treat your foot and ankle needs.
What Is a Broken Toe?
A broken toe occurs when one or more of the toe bones of the foot are broken after an injury. Injuries such as stubbing your toe or dropping a heavy object on it may cause a toe fracture.
Symptoms of a Broken Toe
- Swelling
- Pain (with/without wearing shoes)
- Stiffness
- Nail Injury
Although the injured toe should be monitored daily, it is especially important to have a podiatrist look at your toe if you have severe symptoms. Some of these symptoms include worsening or new pain that is not relieved with medication, sores, redness, or open wounds near the toe.
If you have any questions, please feel free to contact our office located in Pembroke Pines and Plantation, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What to Know About a Broken Toe
The forefoot is composed of five metatarsal bones and fourteen phalanges. Each toe has three phalanges except for the big toe which only has two. Our toes play an essential role to the walking process, which is why a broken toe could seriously disrupt one’s ability to move around. Toe fractures are common and can be very painful. Fortunately, these injuries rarely require surgery and usually heal with rest and a change in activity.
Broken toes typically result from a traumatic event such as falling, stubbing the toe, or dropping something on the toe. Traumatic toe fractures may be categorized as either minor or severe fractures. At times, one may hear a “pop” or “crack” sound when the bone breaks. Common symptoms of a traumatic toe fracture include pain, throbbing, bruising, swelling, and redness.
Another type of toe fractures is a stress fracture. These injuries usually appear in the form of small hairline breaks on the bone. Stress fractures develop after repetitive activity instead of a single injury. Stress fractures occur when the muscles in the bone become too weak to absorb impact. Consequently, the toe bone becomes vulnerable to any pressure and impact it endures. Symptoms for a stress fracture in the toe include swelling without bruising, tenderness to the touch, pain that goes away with rest, and pain after walking or running.
If you suspect that you have a broken toe, you should make an appointment with your podiatrist. He or she will likely diagnose you by performing a physical exam and an X-ray. Treatment for a broken toe may include the R.I.C.E. method, buddy taping, surgery, or antibiotics. The R.I.C.E. method (Rest, Ice, Compression, and Elevation) is a common treatment method for many injuries because it decreases pain. Buddy tapping involves wrapping the injured toe next to an adjacent toe to keep it supported and protected. These two methods have proven to be effective in the healing process for toe fractures. The estimated healing time for a broken toe is approximately four to six weeks. If the injury becomes infected or requires surgery, the estimated healing time may take eight weeks or more.
Cracked Heels and How to Prevent Them
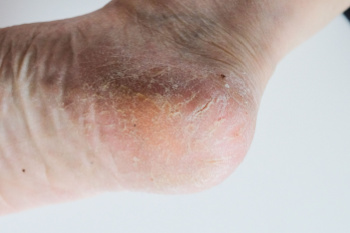
Cracked heels, also known as heel fissures, are characterized by dry, thickened skin on the heels that splits or cracks. This condition often occurs due to factors such as dry weather, excessive standing or walking, improper footwear, or lack of proper foot care. When the skin becomes dry and loses its elasticity, it can crack under pressure, leading to painful fissures that may bleed or become infected, if left untreated. Prevention of cracked heels involves regular moisturizing to keep the skin hydrated and supple. Use a thick, emollient foot cream or lotion containing ingredients like urea or glycerin to help soften and moisturize dry skin. Exfoliating the heels regularly with a pumice stone or foot file can help remove dead skin cells and prevent the buildup of calluses. Additionally, wearing properly fitting shoes with adequate support and cushioning can reduce pressure on the heels and minimize the risk of developing cracked heels. If you have developed cracked heels that persist or become infected, it is strongly suggested that you visit a podiatrist for treatment.
If the skin on your feet starts to crack, you may want to see a podiatrist to find treatment. If you have any concerns, contact Daniel Bell, DPM from Florida. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
It is important to moisturize your cracked heels in order to prevent pain, bleeding, and infection. The reason cracked heels form is because the skin on the foot is too dry to support the immense pressure placed on them. When the foot expands, the dry skin on the foot begins to split.
Ways to Help Heal Them
- Invest in a good foot cream
- Try Using Petroleum Jelly
- Ease up on Soaps
- Drink Plenty of Water
Ways to Prevent Cracked Heels
- Moisturize After Showering
- Skip a Shower
- Keep Shower Water Lukewarm
- Don’t Scrub Your Feet
If you are unsure how to proceed in treating cracked heels, seek guidance from a podiatrist. Your doctor will help you with any questions or information you may need.
If you have any questions, please feel free to contact our office located in Pembroke Pines and Plantation, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels can make life very frustrating and embarrassing when displaying the bare feet. Aside from being unpleasing to the eye, they can also tear stockings and socks and wear out shoes at a faster rate. When severe, cracked heels may cause pain or infection.
Cracked heels are a problem for those who are athletic, those who may walk a lot, and those who have especially dry skin. Those who use medication that dry the skin, those who swim often, wearing certain types of shoes, and those who are diabetic may have trouble with cracked heels. Seniors whose skin produces less oil may also have trouble with cracked feet. There is no one way to develop cracked feet, and there is no cure.
Today, the market consists of numerous products that have a variety of ingredients to promote healing. Some of these are over-the-counter. Others are prescribed by a doctor, especially for those who have chronic dry feet and heels.
Some doctors recommend wearing socks at night for those with rough skin. This helps further healing, and helps creams stay on longer and better absorb into the skin.
One way to alleviate dryness that causes cracked heels is by using moisturizers both day and night. Another way is to make sure the skin is clean and dry at all times. Using a pumice stone to buff away dead skin before putting on moisturizer can also help. Cracked heels will not respond to the cream unless the outer layer of skin is first removed through exfoliation. After exfoliation, lotion or ointment will be absorbed by the skin more easily.
Foods that produce healing and balance can also help the skin from within. Everything that is put into the body can either help it or hurt it. Taking supplements of omega-3 fatty acids and zinc can also be very beneficial.
Nevertheless, not all products are guaranteed to help treat cracked feet. Seeing a professional is best if other treatments options were unsuccessful. A podiatrist should be able to give the best advice to help with this problem.
Flat Feet and Overpronation
 Flat feet, a condition where the arches of the feet touch the ground when you stand, can lead to overpronation. Overpronation occurs when the ankles roll excessively inward with each step during walking or running. This can cause additional strain on the ankles, knees, and hips. Overpronation can also increase the risk of injuries and discomfort due to improper alignment and distribution of body weight. People with flat feet may experience fatigue in their feet and legs, and suffer from pain in the heel or arch area. To help manage symptoms of flat feet and any issues resulting from overpronation, a podiatrist, or foot doctor, may recommend orthotic devices. These are insoles that fit into shoes to provide support for the arches, correct the pronation, and enhance overall foot function. Proper footwear that offers stability and support is also important to effectively manage overpronation. Regular check-ups with a podiatrist can ensure that individuals with flat feet receive the necessary support and guidance to prevent any issues. If you have flat feet, or suspect overpronation when walking, it is suggested you make an appointment with a podiatrist for a full exam and possible gait analysis.
Flat feet, a condition where the arches of the feet touch the ground when you stand, can lead to overpronation. Overpronation occurs when the ankles roll excessively inward with each step during walking or running. This can cause additional strain on the ankles, knees, and hips. Overpronation can also increase the risk of injuries and discomfort due to improper alignment and distribution of body weight. People with flat feet may experience fatigue in their feet and legs, and suffer from pain in the heel or arch area. To help manage symptoms of flat feet and any issues resulting from overpronation, a podiatrist, or foot doctor, may recommend orthotic devices. These are insoles that fit into shoes to provide support for the arches, correct the pronation, and enhance overall foot function. Proper footwear that offers stability and support is also important to effectively manage overpronation. Regular check-ups with a podiatrist can ensure that individuals with flat feet receive the necessary support and guidance to prevent any issues. If you have flat feet, or suspect overpronation when walking, it is suggested you make an appointment with a podiatrist for a full exam and possible gait analysis.
Flatfoot is a condition many people suffer from. If you have flat feet, contact Daniel Bell, DPM from Florida. Our doctor will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact our office located in Pembroke Pines and Plantation, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Flat Feet
Flatfoot is a foot condition in which the arch of the foot has either partially or totally dropped or has never developed. While it is common in babies and small children, it can become a problem for them in adulthood if the arch never forms. For adults, the development of flat feet can be brought upon by injury, as a result of pregnancy due to increased elasticity, or obesity. Those who have health concerns such as rheumatoid arthritis or diabetes may also be at greater risk for developing the condition.
If you suspect that you have flat feet, it is best to consult your podiatrist. Your foot doctor will examine the suspected foot and observe how it looks while you sit and stand. He or she may take an X-ray to determine how serious the condition is. Some common signs of flatfoot include toe drift, in which the toes and front part of the foot point outward, a short Achilles tendon, and a heel that tilts outwardly while the ankle tilts inward.
Once flatfoot has been diagnosed, your podiatrist may suggest one of several treatment options. Flat feet can be rigid, in which the feet appear to have no arch even when the person is not standing; or flexible, in which the person appears to have an arch while not standing, but once standing the arch disappears. Those with flexible flatfoot may be told to reduce any activities that cause pain and to avoid extended periods of walking or standing. Another suggestion may be weight loss, as excessive weight may be placing pressure on the arches
In few cases, if the condition is severe and all other methods have been exhausted surgery may be required. This is normally avoided, however, due to a lengthy recovery time and high cost.
Prescribing Custom-Made Orthotics for Children

Custom-made orthotics are frequently prescribed for children to address various foot and lower limb issues. These specialized shoe inserts are tailored to each child's unique needs, correcting biomechanical imbalances and providing support where necessary. Orthotics may be needed to manage conditions like flat feet, overpronation, or foot deformities, ensuring proper alignment and preventing discomfort or injury. Involving parents in the orthotic prescription process is important for successful treatment. Educating parents about the benefits of orthotics and the importance of compliance ensures they understand their child's needs and can support treatment adherence. Follow-up appointments are critical to monitor progress, make adjustments as needed, and address any concerns. Encouraging compliance in wearing orthotics among children can be facilitated by involving them in the selection process, ensuring comfort and style preferences are considered. Additionally, positive reinforcement, praise for wearing orthotics consistently, and integrating them into daily routines can help foster acceptance and compliance. Fortunately, many children find orthotics comfortable and appreciate the support they provide for their active lifestyles. If your child has foot problems, it is suggested that you schedule an appointment with a podiatrist for diagnosis and care, in addition to discussing whether custom orthotics may provide relief.
If you are having discomfort in your feet and would like to try orthotics, contact Daniel Bell, DPM from Florida. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Are Orthotics?
Orthotics are inserts you can place into your shoes to help with a variety of foot problems such as flat feet or foot pain. Orthotics provide relief and comfort for minor foot and heel pain but can’t correct serious biomechanical problems in your feet.
Over-the-Counter Inserts
Orthotics come in a wide variety of over-the-counter inserts that are used to treat foot pain, heel pain, and minor problems. For example, arch supports can be inserted into your shoes to help correct overarched or flat feet, while gel insoles are often used because they provide comfort and relief from foot and heel pain by alleviating pressure.
Prescription Orthotics
If over-the-counter inserts don’t work for you or if you have a more severe foot concern, it is possible to have your podiatrist prescribe custom orthotics. These high-quality inserts are designed to treat problems such as abnormal motion, plantar fasciitis, and severe forms of heel pain. They can even be used to help patients suffering from diabetes by treating foot ulcers and painful calluses and are usually molded to your feet individually, which allows them to provide full support and comfort.
If you are experiencing minor to severe foot or heel pain, it’s recommended to speak with your podiatrist about the possibilities of using orthotics. A podiatrist can determine which type of orthotic is right for you and allow you to take the first steps towards being pain-free.
If you have any questions please contact our office located in Pembroke Pines and Plantation, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Ankle Foot Orthotics for Athletes
Ankle foot orthotics are shoe inserts that offer support to control the placement and movement of the ankle, correct deformities, and compensate for weakness. These inserts are used to stabilize the foot and ankle and provide toe clearance during the swing phase of gate.
Athletes often suffer foot problems because their feet are not being supported within the shoe. Ankle and foot orthotics are custom made inserts that alleviate stress on the foot. However custom orthotics should be prescribed by a podiatrist who specializes in customized footwear and orthotics design. These inserts are used by athletes for different reasons. Runners use orthotics to absorb shock at heel contact and to set up the forefoot for push-off. Basketball players wear them to control their forefeet while jumping and running.
The two main types of orthotics are over-the-counter orthotics and custom-made orthotics. To be eligible for custom orthotics, an examination of the foot and ankle will need to be completed. Afterward, both the foot and ankle will need to be casted and fitted for the proper orthotic. When the fitting process is complete, adjustments can be made to make sure everything fits perfectly.
Over the counter orthotics tend to be more popular than custom fit ones. Athletes who have less severe aches and pains in the foot, ankle or lower back area can use the over-the-counter version of orthotics. Unfortunately, over-the-counter orthotics tend to not work in treating severe injuries or ailments. Whenever you suspect you may need an ankle foot orthotic, you should consult with your podiatrist to determine which type of orthotic is right for you.
Recovering From an Ankle Sprain

An ankle sprain, though common, can be a real setback, disrupting mobility and causing discomfort. It occurs when the ligaments that support the ankle are stretched or torn, often due to sudden twisting or rolling movements. Symptoms can include pain, swelling, bruising, and difficulty bearing weight on the affected ankle. Recovery from an ankle sprain typically involves rest, compression, and elevation to reduce swelling and pain. Additionally, gradually reintroducing weight-bearing activities and performing gentle exercises to restore strength and flexibility can also help. However, recurrent sprains can indicate underlying issues like weakened ligaments or poor ankle stability. If you have sustained an ankle sprain, it is suggested that you schedule an appointment with a podiatrist for a proper diagnosis and tailored treatment plan.
Ankle sprains are common but need immediate attention. If you need your feet checked, contact Daniel Bell, DPM from Florida. Our doctor can provide the care you need to keep you pain-free and on your feet.
How Does an Ankle Sprain Occur?
Ankle sprains take place when the ligaments in your ankle are torn or stretched beyond their limits. There are multiple ways that the ankle can become injured, including twisting or rolling over onto your ankle, putting undue stress on it, or causing trauma to the ankle itself.
What Are the Symptoms?
- Mild to moderate bruising
- Limited mobility
- Swelling
- Discoloration of the skin (depending on severity)
Preventing a Sprain
- Wearing appropriate shoes for the occasion
- Stretching before exercises and sports
- Knowing your limits
Treatment of a Sprain
Treatment of a sprain depends on the severity. Many times, people are told to rest and remain off their feet completely, while others are given an air cast. If the sprain is very severe, surgery may be required.
If you have suffered an ankle sprain previously, you may want to consider additional support such as a brace and regular exercises to strengthen the ankle.
If you have any questions please feel free to contact our office located in Pembroke Pines and Plantation, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Blog Archives
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021