Connect With Us
Blog

Prescribing Custom-Made Orthotics for Children

Custom-made orthotics are frequently prescribed for children to address various foot and lower limb issues. These specialized shoe inserts are tailored to each child's unique needs, correcting biomechanical imbalances and providing support where necessary. Orthotics may be needed to manage conditions like flat feet, overpronation, or foot deformities, ensuring proper alignment and preventing discomfort or injury. Involving parents in the orthotic prescription process is important for successful treatment. Educating parents about the benefits of orthotics and the importance of compliance ensures they understand their child's needs and can support treatment adherence. Follow-up appointments are critical to monitor progress, make adjustments as needed, and address any concerns. Encouraging compliance in wearing orthotics among children can be facilitated by involving them in the selection process, ensuring comfort and style preferences are considered. Additionally, positive reinforcement, praise for wearing orthotics consistently, and integrating them into daily routines can help foster acceptance and compliance. Fortunately, many children find orthotics comfortable and appreciate the support they provide for their active lifestyles. If your child has foot problems, it is suggested that you schedule an appointment with a podiatrist for diagnosis and care, in addition to discussing whether custom orthotics may provide relief.
If you are having discomfort in your feet and would like to try orthotics, contact Daniel Bell, DPM from Florida. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Are Orthotics?
Orthotics are inserts you can place into your shoes to help with a variety of foot problems such as flat feet or foot pain. Orthotics provide relief and comfort for minor foot and heel pain but can’t correct serious biomechanical problems in your feet.
Over-the-Counter Inserts
Orthotics come in a wide variety of over-the-counter inserts that are used to treat foot pain, heel pain, and minor problems. For example, arch supports can be inserted into your shoes to help correct overarched or flat feet, while gel insoles are often used because they provide comfort and relief from foot and heel pain by alleviating pressure.
Prescription Orthotics
If over-the-counter inserts don’t work for you or if you have a more severe foot concern, it is possible to have your podiatrist prescribe custom orthotics. These high-quality inserts are designed to treat problems such as abnormal motion, plantar fasciitis, and severe forms of heel pain. They can even be used to help patients suffering from diabetes by treating foot ulcers and painful calluses and are usually molded to your feet individually, which allows them to provide full support and comfort.
If you are experiencing minor to severe foot or heel pain, it’s recommended to speak with your podiatrist about the possibilities of using orthotics. A podiatrist can determine which type of orthotic is right for you and allow you to take the first steps towards being pain-free.
If you have any questions please contact our office located in Pembroke Pines and Plantation, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Ankle Foot Orthotics for Athletes
Ankle foot orthotics are shoe inserts that offer support to control the placement and movement of the ankle, correct deformities, and compensate for weakness. These inserts are used to stabilize the foot and ankle and provide toe clearance during the swing phase of gate.
Athletes often suffer foot problems because their feet are not being supported within the shoe. Ankle and foot orthotics are custom made inserts that alleviate stress on the foot. However custom orthotics should be prescribed by a podiatrist who specializes in customized footwear and orthotics design. These inserts are used by athletes for different reasons. Runners use orthotics to absorb shock at heel contact and to set up the forefoot for push-off. Basketball players wear them to control their forefeet while jumping and running.
The two main types of orthotics are over-the-counter orthotics and custom-made orthotics. To be eligible for custom orthotics, an examination of the foot and ankle will need to be completed. Afterward, both the foot and ankle will need to be casted and fitted for the proper orthotic. When the fitting process is complete, adjustments can be made to make sure everything fits perfectly.
Over the counter orthotics tend to be more popular than custom fit ones. Athletes who have less severe aches and pains in the foot, ankle or lower back area can use the over-the-counter version of orthotics. Unfortunately, over-the-counter orthotics tend to not work in treating severe injuries or ailments. Whenever you suspect you may need an ankle foot orthotic, you should consult with your podiatrist to determine which type of orthotic is right for you.
Recovering From an Ankle Sprain

An ankle sprain, though common, can be a real setback, disrupting mobility and causing discomfort. It occurs when the ligaments that support the ankle are stretched or torn, often due to sudden twisting or rolling movements. Symptoms can include pain, swelling, bruising, and difficulty bearing weight on the affected ankle. Recovery from an ankle sprain typically involves rest, compression, and elevation to reduce swelling and pain. Additionally, gradually reintroducing weight-bearing activities and performing gentle exercises to restore strength and flexibility can also help. However, recurrent sprains can indicate underlying issues like weakened ligaments or poor ankle stability. If you have sustained an ankle sprain, it is suggested that you schedule an appointment with a podiatrist for a proper diagnosis and tailored treatment plan.
Ankle sprains are common but need immediate attention. If you need your feet checked, contact Daniel Bell, DPM from Florida. Our doctor can provide the care you need to keep you pain-free and on your feet.
How Does an Ankle Sprain Occur?
Ankle sprains take place when the ligaments in your ankle are torn or stretched beyond their limits. There are multiple ways that the ankle can become injured, including twisting or rolling over onto your ankle, putting undue stress on it, or causing trauma to the ankle itself.
What Are the Symptoms?
- Mild to moderate bruising
- Limited mobility
- Swelling
- Discoloration of the skin (depending on severity)
Preventing a Sprain
- Wearing appropriate shoes for the occasion
- Stretching before exercises and sports
- Knowing your limits
Treatment of a Sprain
Treatment of a sprain depends on the severity. Many times, people are told to rest and remain off their feet completely, while others are given an air cast. If the sprain is very severe, surgery may be required.
If you have suffered an ankle sprain previously, you may want to consider additional support such as a brace and regular exercises to strengthen the ankle.
If you have any questions please feel free to contact our office located in Pembroke Pines and Plantation, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Three Grades of Ankle Sprains
An ankle sprain occurs when one or more ankle ligament gets overly stretched. Ligaments are strong bands of tissue that bind and support the bones and other structures that make up the ankle. In more severe ankle sprains, the ligament(s) tear—either partially or completely—and there may be an audible popping noise at the moment of injury.
Ankle sprains are quite common and can occur when the ankle rolls outwardly (eversion) or inwardly (inversion), causing the ligament(s) to stretch beyond normal limits, or even tear. Falls, twists, or blows to the ankle during sports or other activities can cause this injury, as well as wearing improper footwear, running on uneven surfaces, or having weak ankles.
Depending on the injury’s severity, an ankle sprain will be classified as Grade I, Grade II, or Grade III. Grade I sprains involve ligament(s) being overly stretched but not torn, with symptoms of mild pain, swelling, and ankle instability. There may also be some difficulty bearing weight. A Grade II sprain usually involves a partial tear of the ligament which brings more intensity in these symptoms, along with possible bruising. With a Grade III sprain, the ligament is completely torn, the symptoms are severe, and it may not be possible to put weight on the affected foot at all.
To diagnose and grade an ankle sprain, a podiatrist will perform a physical examination, checking for tenderness and range of motion in the ankle. For more severe sprains, X-rays or other imaging studies may be necessary.
It is vitally important to have an ankle sprain treated properly as improper healing often leads to future ankle sprains and possibly even chronic ankle stability. Treatment for an ankle sprain will vary, depending on its severity, and may include the RICE method (Rest/Ice/Compression/Elevation), physical therapy, bracing, medications, and possibly even surgery to repair a torn ligament. Rehabilitation is very important for the sprain to heal properly and to restore functionality.
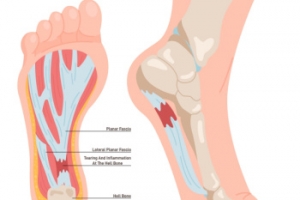
Symptoms of Plantar Fasciitis
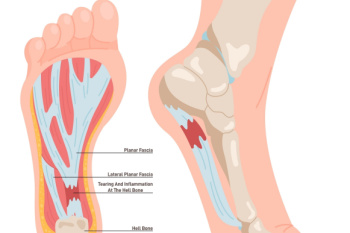
Plantar fasciitis can be a result of inflammation of the plantar fascia, which is the thick band of tissue connecting the heel to the toes. This condition typically occurs from repetitive strain or excessive pressure on the feet. It is commonly experienced by athletes, runners, and individuals who stand for extended periods. The hallmark symptom of plantar fasciitis is heel pain that is particularly sharp and stabbing, and often worsens with activity or after prolonged periods of rest. Additionally, individuals with plantar fasciitis may experience discomfort along the arch of the foot. While the severity of symptoms can vary, untreated plantar fasciitis can significantly impair mobility and quality of life. Early recognition and appropriate management, including rest, stretching exercises, orthotic devices, and in severe cases, surgical intervention, are important for effective relief and prevention of long-term complications. Plantar fasciitis is treated by a podiatrist. If you are experiencing any of the above symptoms, it is suggested that you contact this type of doctor who can successfully provide treatment.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Daniel Bell, DPM from Florida. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our office located in Pembroke Pines and Plantation, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
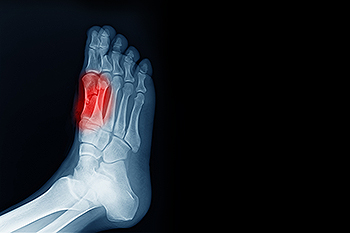
Causes of Broken Heels

Understanding the causes of a broken heel helps in recognizing the signs and seeking appropriate treatment. Fractures in the heel often result from significant force, such as falling from a height, a car accident, or a sports injury. Repetitive stress on the heel, which may develop from long-distance running, can lead to stress fractures in the heel. Symptoms of heel fractures include pain when touching and putting weight on it. Swelling and difficulty walking normally are other symptoms. A fracture of the heel bone may also cause internal bleeding, resulting in bruising after a day or so. To diagnose a broken heel, a podiatrist employs X-rays and sometimes CT scans. Treatment may involve wearing a cast or splint. Surgical intervention for severe cases and the use of assistive devices like canes and protective footwear during recovery may be prescribed. If you suspect a broken heel, it's suggested that you make an appointment with a podiatrist for proper evaluation and personalized care.
A broken foot requires immediate medical attention and treatment. If you need your feet checked, contact Daniel Bell, DPM from Florida. Our doctor can provide the care you need to keep you pain-free and on your feet.
Broken Foot Causes, Symptoms, and Treatment
A broken foot is caused by one of the bones in the foot typically breaking when bended, crushed, or stretched beyond its natural capabilities. Usually the location of the fracture indicates how the break occurred, whether it was through an object, fall, or any other type of injury.
Common Symptoms of Broken Feet:
- Bruising
- Pain
- Redness
- Swelling
- Blue in color
- Numbness
- Cold
- Misshapen
- Cuts
- Deformities
Those that suspect they have a broken foot shoot seek urgent medical attention where a medical professional could diagnose the severity.
Treatment for broken bones varies depending on the cause, severity and location. Some will require the use of splints, casts or crutches while others could even involve surgery to repair the broken bones. Personal care includes the use of ice and keeping the foot stabilized and elevated.
If you have any questions please feel free to contact our office located in Pembroke Pines and Plantation, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Causes, Symptoms, and Treatment for a Broken Foot
The human foot has 26 different bones, and the foot is divided into three parts: the hindfoot, the midfoot, and the forefoot. Each section of the foot is composed of a different amount of bones. For instance, the forefoot is made up of 19 bones. The midfoot is composed of five smaller bones called the navicular, cuboid, and three cuneiform bones. Lastly, the hindfoot is made up of only the talus and the calcaneus. The feet tend to be vulnerable to slipping and twisting; consequently, fractured bones within the foot are common. When a bone gets crushed, bent, twisted, or stretched it may become broken.
Many foot fractures occur through an accident or trauma. More specifically, common causes for broken feet are car accidents, falls, missteps, or overuse. If you have a broken ankle or foot, you may have one or more of the following symptoms: throbbing pain, swelling, bruising, tenderness, deformities, and difficulty walking.
There are some factors that may put you at a higher risk of developing a broken foot. People who participate in high-impact sports are more likely to develop foot fractures because of the stresses, direct blows, and twisting injuries involved in gameplay. Additionally, those who suddenly increase their activity level are more likely to suffer a stress fracture.
Unfortunately, there are different complications that may arise because of a foot fracture. For instance, arthritis may be caused by fractures that extend into the joints. Bone infections are also possible in open fractures due to the bone being exposed to bacteria. However, there are ways you can help prevent yourself from breaking your foot. One way to avoid fractures is to wear proper footwear. If you plan on going on a run, you should wear running shoes. You should also replace your shoes if you notice that they are becoming worn out. For runners, it is best to replace shoes every 300 to 400 miles.
Treatment for foot fractures usually consists of rest, ice, elevation, and compression (RICE). If you plan on wrapping your foot, try not to wrap it too tightly because doing so may cut off blood supply in the foot. You should also avoid walking on the fractured foot.
If you suspect you have a broken foot, you should see your podiatrist right away. It is important that you have someone bring you to your doctor, since driving with a broken foot can be dangerous. You should especially seek urgent care if you are experiencing numbness, pain, or deformities in your foot.
Are Bunions Affecting Your Everyday Life?
Diagnosis and Treatment of Sesamoiditis
Sesamoiditis is a painful condition that affects the tendons around two small bones in the foot. These specialized bones, known as sesamoids, are unique in that they connect to muscles via tendons rather than to other bones. Typically, tendons become inflamed often due to overuse or repeated trauma, causing inflammation. This causes pain beneath the ball of the foot that gradually intensifies and may cause swelling or bruising. Certain activities, like running, basketball, or ballet, which impose considerable pressure on the ball of the foot, heighten the risk of developing sesamoiditis. Diagnosis involves a thorough physical examination to assess tenderness and limitations in mobility. A podiatrist will order imaging studies, such as X-rays, MRI scans, or ultrasounds to confirm the diagnosis and evaluate the extent of the condition. Treatment primarily focuses on lifestyle modifications, including modifying activity and changes in footwear. Pain management strategies such as custom orthotics and certain medications may also be prescribed. In severe cases where conservative measures fail, surgery may be necessary. If you are experiencing symptoms of sesamoiditis, it is suggested that you schedule an appointment with a podiatrist.
Sesamoiditis is an unpleasant foot condition characterized by pain in the balls of the feet. If you think you’re struggling with sesamoiditis, contact Daniel Bell, DPM of Florida. Our doctor will treat your condition thoroughly and effectively.
Sesamoiditis
Sesamoiditis is a condition of the foot that affects the ball of the foot. It is more common in younger people than it is in older people. It can also occur with people who have begun a new exercise program, since their bodies are adjusting to the new physical regimen. Pain may also be caused by the inflammation of tendons surrounding the bones. It is important to seek treatment in its early stages because if you ignore the pain, this condition can lead to more serious problems such as severe irritation and bone fractures.
Causes of Sesamoiditis
- Sudden increase in activity
- Increase in physically strenuous movement without a proper warm up or build up
- Foot structure: those who have smaller, bonier feet or those with a high arch may be more susceptible
Treatment for sesamoiditis is non-invasive and simple. Doctors may recommend a strict rest period where the patient forgoes most physical activity. This will help give the patient time to heal their feet through limited activity. For serious cases, it is best to speak with your doctor to determine a treatment option that will help your specific needs.
If you have any questions please feel free to contact our office located in Pembroke Pines and Plantation, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Blog Archives
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021