Connect With Us
Blog

Dealing With Athlete’s Foot

Athlete’s foot, medically known as tinea pedis, is a fungal infection that is not limited to athletes. Anyone can contract the infection if exposed to the highly contagious fungi, known as dermatophytes, that cause it. The most common symptom of athlete’s foot is an itching and burning sensation between the toes or on the bottom of the foot, along with a scaly rash. You may also experience painful cracking of the skin, blistering, and thickening on the soles of the foot. While athlete’s foot is not considered to be dangerous, it can result in a secondary infection if bacteria enter the broken skin. The main complication of having athlete’s foot is infecting other parts of the body that have touched your feet. In addition, anyone sharing personal items or showering spaces with you is at increased risk of infection. Athlete’s foot is treatable with anti-fungal creams, lotions, powders, and sprays. If symptoms persist after a few weeks, please consult a podiatrist who can examine the infected area and prescribe medications or creams that are more potent.
Athlete’s foot is an inconvenient condition that can be easily reduced with the proper treatment. If you have any concerns about your feet and ankles, contact Daniel Bell, DPM from Florida. Our doctor will treat your foot and ankle needs.
Athlete’s Foot: The Sole Story
Athlete's foot, also known as tinea pedis, can be an extremely contagious foot infection. It is commonly contracted in public changing areas and bathrooms, dormitory style living quarters, around locker rooms and public swimming pools, or anywhere your feet often come into contact with other people.
Solutions to Combat Athlete’s Foot
- Hydrate your feet by using lotion
- Exfoliate
- Buff off nails
- Use of anti-fungal products
- Examine your feet and visit your doctor if any suspicious blisters or cuts develop
Athlete’s foot can cause many irritating symptoms such as dry and flaking skin, itching, and redness. Some more severe symptoms can include bleeding and cracked skin, intense itching and burning, and even pain when walking. In the worst cases, Athlete’s foot can cause blistering as well. Speak to your podiatrist for a better understanding of the different causes of Athlete’s foot, as well as help in determining which treatment options are best for you.
If you have any questions please feel free to contact our office located in Pembroke Pines and Plantation, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Athlete’s Foot
Athlete’s foot, or tinea pedis, is a skin disease caused by a fungal infection. The infection typically occurs between the toes, and the feet are most subject to this disease because shoes best create the warm, dark, and moist environment in which fungus thrives. Other areas that create a similar environment, such as swimming pools, public showers, and locker rooms; can also promote fungi growth.
Symptoms of athlete’s foot include dry skin, itching, scaling, inflammation, and blistering. Sometimes, blisters can evolve into the cracks or breaks in the skin. The exposed tissue can then create pain, swelling, and discharge. The spread of infection can cause itching and burning as well.
While athlete’s foot commonly occurs between the toes, it may also spread to the toenails or soles of the feet. Other parts of the body, such as the groin or underarms, can also become infected if they are touched after the original area of infection is scratched. Aside from physical contact, athlete’s foot can also spread through the contamination of footwear, clothing or bedsheets.
Proper foot hygiene is essential in preventing athlete’s foot. You can prevent the fungus from spreading by frequently washing your feet using soap and water, thoroughly drying the feet between the toes, changing shoes and socks every day to reduce moisture, and ensuring that bathroom and shower floors are disinfected. Other tips include using shower shoes, avoiding walking barefoot in public environments, wearing light and airy shoes, and wearing socks that keep the feet dry.
While treatment for athlete’s foot can involve topical or oral antifungal drugs, mild cases of the infection can be treated by dusting foot powder in shoes and socks. Any treatment used can be supplemented by frequently bathing the feet and drying the toes. If proper foot hygiene and self-care do not ease your case of athlete’s foot, contact your podiatrist. He will determine if the underlying cause of your condition is truly a fungus. If that is the case, a comprehensive treatment plan may be suggested with the inclusion of prescription antifungal medications.
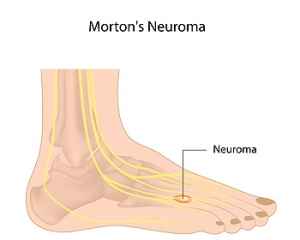
Morton’s Neuroma Surgery

Sometimes, certain afflictions of the foot can be so severe that they can only be treated properly by undergoing a kind of surgical procedure. It is important to note that foot surgery is not for everyone and you may not be a good candidate for particular surgical procedures. However, sometimes undergoing a surgical procedure can be beneficial and it might be the only way to treat severe conditions. For example, some individuals can benefit from a surgical procedure for Morton’s neuroma. This condition is defined as the swelling or inflammation of the nerve between the toes or metatarsal bones. The surgical procedure to address Morton’s neuroma consists of removing a small section of the nerve. An incision must be made to get to the damaged nerve and then the skin is quickly sewn up following the removal of the nerve. Contact a podiatrist today for more information about Morton’s neuroma or to learn if you might be a good candidate for surgery.
Foot surgery is sometimes necessary to treat a foot ailment. To learn more, contact Daniel Bell, DPM of Florida. Our doctor will assist you with all of your foot and ankle needs.
When Is Surgery Necessary?
Foot and ankle surgery is generally reserved for cases in which less invasive, conservative procedures have failed to alleviate the problem. Some of the cases in which surgery may be necessary include:
- Removing foot deformities like bunions and bone spurs
- Severe arthritis that has caused bone issues
- Cosmetic reconstruction
What Types of Surgery Are There?
The type of surgery you receive will depend on the nature of the problem you have. Some of the possible surgeries include:
- Bunionectomy for painful bunions
- Surgical fusion for realignment of bones
- Neuropathy decompression surgery to treat nerve damage
Benefits of Surgery
Although surgery is usually a last resort, it can provide more complete pain relief compared to non-surgical methods and may allow you to finally resume full activity.
Surgical techniques have also become increasingly sophisticated. Techniques like endoscopic surgery allow for smaller incisions and faster recovery times.
If you have any questions please feel free to contact our office located in Pembroke Pines and Plantation, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Foot Surgery
In most cases, foot surgery is often chosen as the last available option for conditions that have otherwise been unsuccessfully treated. Surgery may be necessary for several reasons, including the removal of foot deformities (e.g. bone spurs or bunions), arthritis problems, reconstruction due to injury, and congenital malformations (e.g. club foot or flat feet). Regardless of one’s age, foot surgery may be the only successful option for treatment for certain conditions.
The type of surgery one undergoes depends on the type of foot condition the patient has. For the removal of a bunion growth, a bunionectomy is necessary. If the bones in the feet need to be realigned or fused together, a surgical fusion of the foot is needed. For pain or nerve issues, a patient may require surgery in which the tissues surrounding the painful nerve are removed. Initially, less invasive treatments are generally attempted; surgery is often the last measure taken if other treatments are unsuccessful.
While in many cases surgery is often deemed as the final resort, choosing surgery comes with certain benefits. The associated pain experienced in relation to the particular condition is often relieved with surgery, allowing patients to quickly resume daily activities. The greatest benefit, however, is that surgery generally eliminates the problem immediately.
Podiatry history has shown that foot treatments continue to evolve over time. In the field of foot surgery, endoscopic surgery is just one of the many advanced forms of surgery. As technology vastly improves so too will the various techniques in foot surgery, which already require smaller and smaller incisions with the use of better and more efficient tools. Thanks to such innovations, surgery is no longer as invasive as it was in the past, allowing for faster and easier recoveries.
Why Do Cracked Heels Occur?

People who have cracked heels may notice they become worse in the colder months. This condition can cause your feet to look older and may be painful or uncomfortable. There are various reasons why cracked heels can develop, including standing on hard surfaces and wearing shoes that have an open back. Flip flops and sandals also fall into this category and if you choose to wear this shoe, it helps if it has a strap to secure the heel. People who are obese may find they have cracked heels due to the added weight the heels endure. Medical conditions like eczema, psoriasis, and thyroid disorders may lead to cracked heels. Some of the symptoms that are associated with this ailment include redness, flaky skin, and in severe cases, the cracks in the heel may bleed causing an infection. There are several treatment methods for cracked heels and if you suffer from this condition, it is advised that you consult a podiatrist who can help you with effective healing techniques.
If the skin on your feet starts to crack, you may want to see a podiatrist to find treatment. If you have any concerns, contact Daniel Bell, DPM from Florida. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
It is important to moisturize your cracked heels in order to prevent pain, bleeding, and infection. The reason cracked heels form is because the skin on the foot is too dry to support the immense pressure placed on them. When the foot expands, the dry skin on the foot begins to split.
Ways to Help Heal Them
- Invest in a good foot cream
- Try Using Petroleum Jelly
- Ease up on Soaps
- Drink Plenty of Water
Ways to Prevent Cracked Heels
- Moisturize After Showering
- Skip a Shower
- Keep Shower Water Lukewarm
- Don’t Scrub Your Feet
If you are unsure how to proceed in treating cracked heels, seek guidance from a podiatrist. Your doctor will help you with any questions or information you may need.
If you have any questions, please feel free to contact our office located in Pembroke Pines and Plantation, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels can make life very frustrating and embarrassing when displaying the bare feet. Aside from being unpleasing to the eye, they can also tear stockings and socks and wear out shoes at a faster rate. When severe, cracked heels may cause pain or infection.
Cracked heels are a problem for those who are athletic, those who may walk a lot, and those who have especially dry skin. Those who use medication that dry the skin, those who swim often, wearing certain types of shoes, and those who are diabetic may have trouble with cracked heels. Seniors whose skin produces less oil may also have trouble with cracked feet. There is no one way to develop cracked feet, and there is no cure.
Today, the market consists of numerous products that have a variety of ingredients to promote healing. Some of these are over-the-counter. Others are prescribed by a doctor, especially for those who have chronic dry feet and heels.
Some doctors recommend wearing socks at night for those with rough skin. This helps further healing, and helps creams stay on longer and better absorb into the skin.
One way to alleviate dryness that causes cracked heels is by using moisturizers both day and night. Another way is to make sure the skin is clean and dry at all times. Using a pumice stone to buff away dead skin before putting on moisturizer can also help. Cracked heels will not respond to the cream unless the outer layer of skin is first removed through exfoliation. After exfoliation, lotion or ointment will be absorbed by the skin more easily.
Foods that produce healing and balance can also help the skin from within. Everything that is put into the body can either help it or hurt it. Taking supplements of omega-3 fatty acids and zinc can also be very beneficial.
Nevertheless, not all products are guaranteed to help treat cracked feet. Seeing a professional is best if other treatments options were unsuccessful. A podiatrist should be able to give the best advice to help with this problem.
Foot and Ankle Injuries From Falling

The feet and ankles are commonly affected during falls. Frequent foot injuries caused by falls can include strains, sprained ankles, fractured bones, or even torn Achilles tendons. Because pressure is still applied to the foot, even when casted, it is challenging to fully immobilize the foot and ankle, making the healing process somewhat slow. Such injuries can alter one’s enjoyment and quality of life, and lead to chronic pain. If you have sustained a foot or ankle injury in a fall, contact a podiatrist who can correctly diagnose the problem and get you on the road to recovery as quickly as possible.
Preventing falls among the elderly is very important. If you are older and have fallen or fear that you are prone to falling, consult with Daniel Bell, DPM from Florida. Our doctor will assess your condition and provide you with quality advice and care.
Every 11 seconds, an elderly American is being treated in an emergency room for a fall related injury. Falls are the leading cause of head and hip injuries for those 65 and older. Due to decreases in strength, balance, senses, and lack of awareness, elderly persons are very susceptible to falling. Thankfully, there are a number of things older persons can do to prevent falls.
How to Prevent Falls
Some effective methods that older persons can do to prevent falls include:
- Enrolling in strength and balance exercise program to increase balance and strength
- Periodically having your sight and hearing checked
- Discuss any medications you have with a doctor to see if it increases the risk of falling
- Clearing the house of falling hazards and installing devices like grab bars and railings
- Utilizing a walker or cane
- Wearing shoes that provide good support and cushioning
- Talking to family members about falling and increasing awareness
Falling can be a traumatic and embarrassing experience for elderly persons; this can make them less willing to leave the house, and less willing to talk to someone about their fears of falling. Doing such things, however, will increase the likelihood of tripping or losing one’s balance. Knowing the causes of falling and how to prevent them is the best way to mitigate the risk of serious injury.
If you have any questions, please feel free to contact our office located in Pembroke Pines and Plantation, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Falls Prevention
Elderly Americans are very susceptible to falls as they get older. Everyone experiences decreases in flexibility, balance, strength, and the senses as they age. This correlates to some eye-opening statistics. 1 in 4 Americans aged 65 and older fall each year. An elderly American is being treated for a fall in an emergency room every 11 seconds. In light of these striking statistics, one can see the importance of taking steps to prevent falls.
Finding an exercise program for the elderly is an excellent way to reduce the likelihood of falls. Look for an exercise program that improves strength and balance. Elderly people who live a more sedentary lifestyle, with little physical activity, are at an increased risk of falling. Wearing well-fitted footwear that provides good foot support and cushion will help prevent falls from poorly fitted shoes. Talking to a podiatrist about your susceptibility to falls and about inspecting your prescriptions will help to avoid any medication that could make falls more likely. Due to a decline in the senses among the elderly, having your eyes and hearing checked is recommended.
Around half of all falls occur in the household. Removing tripping hazards in the home and making it more accommodating to older persons can significantly reduce falls. Some notable household changes include increasing lighting around the house, installing grab bars in the shower and bathroom, and making sure the floor is clear of clutter. Other smart options include installing a shower chair, using rubber-bottomed rugs, and placing railings on both sides of stairwells.
Finally, discuss with a doctor and your family about your fear of falling. This will help to increase awareness among the population on the need for fall prevention. A lack of awareness on the matter, and a downplaying of importance are what increase the risks of falling. Following these tips can help to reduce the risk for yourself and your loved ones.
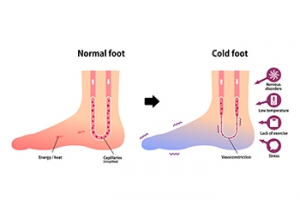
Cold Feet After Exercising

If your feet feel cold during or right after exercising, when the rest of your body feels warm, it may be a sign that something is wrong. It can be as simple as wearing shoes or socks that are too tight and restrict proper blood flow to the feet. Cold feet after exercising may also be caused by more serious underlying conditions, such as diabetes or peripheral artery disease. Falling or bumping into something during exercise also may cause the feet to become cold. In addition, fractures, bone spurs, or cysts may cause numbness and cold feet. Whatever the cause, having cold feet after exercise is not something to ignore. First, check your footwear to make sure it fits properly and is not laced too tightly. Next, check your feet for any sores or cuts that may have formed. If ignored, these can turn into ulcers. Foot cramps at night or pain that gets worse if your feet are elevated can also be warning signs. If getting cold feet after exercising becomes a common occurrence, it may be wise to visit a podiatrist for an exam, a diagnosis, and a treatment plan.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Daniel Bell, DPM from Florida. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our office located in Pembroke Pines and Plantation, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blog Archives
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021